Review Article- Asian Journal of Pharmaceutical Technology and Innovation(2018)
Sterilization in Dental Practice – A Review
Suvarna V Biradar*Dr. Suvarna V Biradar, Senior Lecturer, Department of Public Health Dentistry, HKDET’S Dental College Hospital & Research Institute, Humnabad 585330. Bidar, Karnataka, India, Tel: +918970831926, Email: suvarna13gulbarga@gmail.com
Received: 10-Jan-2018 Accepted Date: Jan 18, 2018 ; Published: 20-Jan-2018
Abstract
In Dentistry, critical instruments are those used to penetrate soft tissue or bone, or enter into or contact the bloodstream or other normally sterile tissue. They should be sterilized after each use. Sterilization is achieved by various methods. Traditional sterilization methods are often time consuming for practical use. Today's sterilizers are sophisticated, automatic, and computerized devices that accurately execute programmed jobs, creating uniform conditions inside pressure vessels to achieve sterilization. Specialized knowledge is necessary to ensure that the right cycle is selected; this requires an educated and competent operator. Sterilization practices, standards and products are changing in the health care system and continues to undergo dramatic restructuring. The causes of this restructuring are hospital consolidations, implementation of diagnosticrelated- group reimbursement, cost-containment programs, and increasing acceptance of disposable packs.
Keywords
Autoclave, Hot air oven, Disinfection, SterilizationIntroduction
Micro-organisms are ubiquitous. Since they cause contamination and infection, it becomes necessary to remove or destroy them from the materials or from areas. This is the purpose of sterilization.The purpose of sterilization in microbiology to prevent contamination by the organisms, in surgery to maintain asepsis, in food and drug manufacture to ensure safety from the contaminating organisms and in many other situations.The instruments used in medical field and the dental instruments used in the dental field will be contaminated with the blood, body fluids etc during the clinical procedures, which will be cleaned and sterilized by different methods of sterilization. This reduces the chances of infection between doctors-patients, patient-dentist, dentist-patient and between patient to patient. Hence, sterilization plays a significant role in the field of health care.
Sterilization
DEFINITION
“STERILIZATION IS A PROCESS WHEREBY ALL FORMS OF MICROBIAL LIFE INCLUDING BACTERIAL SPORES ARE KILLED”
IT CAN BE ACCOMPLISHED BY PHYSICAL OR CHEMICAL MEANS
( SOURCE : BAILEY AND SCOTT’S DIAGNOSTIC MICROBIOLOGY 10TH EDITION PG.NO.20)
“IT IS THE PROCESS BY WHICH AN ARTICLE, SURFACE OR THE MEDIUM IS MADE FREE OF ALL MICRO-ORGANISMS EITHER IN THE VEGETATIVE OR SPORE FORM”
( SOURCE : ANANTHANARAYAN & PANIKER’S TEXTBOOK OF MICROBIOLOGY 8TH EDITION PG.NO.30-38)
A sterility requirement for medical products means that a living organism will be present on an object after the sterilizing process is equal to or less than one in a million, so called Sterility Assurance Level (SAL) = 10 degree DISINFECTION
“DISINFECTION IS A PROCESS WHEREBY PATHOGENIC ORGANISMS, BUT NOT NECESSARILY ALL MICRO-ORGANISMS OR SPORES ARE DESTROYED”
(SOURCE : BAILEY AND SCOTT’S DIAGNOSTIC MICROBIOLOGY 10TH EDITION PG.NO.20-22)
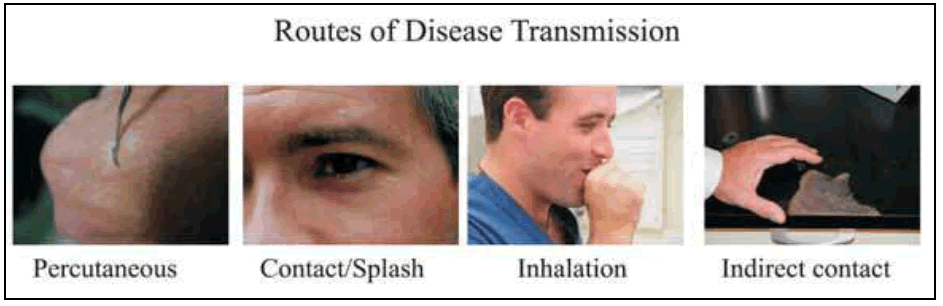
Routes of Disease Transmission
Routes of disease transmission can be specific to various fields of healthcare. In dentistry, diseases can be transmitted from patient-to-patient, dentist to patient, and patient to dentist when adequate precautions are not followed. Dental Healthcare Workers and patients can further transmit the diseases to their respective families and friends. Common modes of disease transmission in the order of severity are :
Percutaneous (high risk)
• Inoculation of microbes from blood and saliva transmitted through needles and sharps Contact (high risk)
• Touching or exposing non-intact skin to infective oral lesions, infected tissue surfaces or infected fluids, splash and spatter of infected fluids
Inhalation of Aerosols or droplets containing pathogens (moderate risk)
• Breathing bioaerosols suspended in the clinics ambient air laden with infective material while using handpieces and scalers or droplet nucleii from coughing
Indirect contact through fomites (low risk)
• Touching contaminated inanimate surfaces in the dental treatment room or operatory
NOTE : ACCIDENTAL SELF INJURY WITH A CONTAMINATED NEEDLE OR SHARP INSTRUMENTS WILL LEAD TO THE TRANSMISSION OF VARIOUS MICRO-ORGANISMS SUCH AS :
❏ HEPATITIS B VIRUS
❏ HEPATITIS C VIRUS
❏ HEPATITIS D VIRUS
❏ HERPES SIMPLEX VIRUS I
❏ HERPES SIMPLEX VIRUS II
❏ HUMAN IMMUNODEFICIENCY VIRUS
❏ CLOSTRIDIUM TETANI
INFECTION CONTROL
Dentistry is predominantly a field of surgery, involving exposure to blood and other potentially infectious materials, and therefore, requires a high standard of Infection Control and Safety practice in controlling cross contamination and occupational exposures to blood-borne diseases. Apart from blood-borne diseases such as Hepatitis B infection and HIV infections, the dental health care workers are potentially at risk of acquiring respiratory diseases, childhood diseases, sexually transmitted diseases commonly encountered in dentistry. The infection can be controlled by the use of personal protective equipments and also by controlling the infection at the clinical working area.
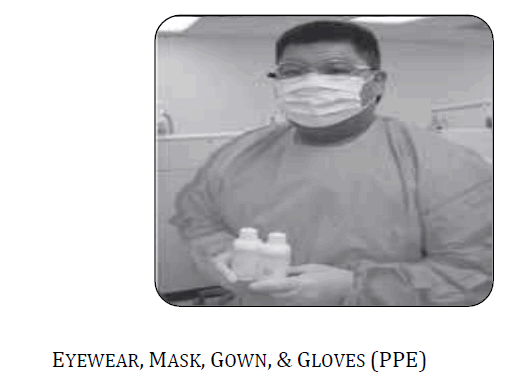
PERSONAL PROTECTIVE EQUIPMENT
AREA OF INFECTION CONTROL
Personal Protective Equipment
Personal Protective Equipment (PPE) commonly used in general dental care are single-use-disposable gloves (sterile or non-sterile), protective eyewear, face-shields, masks, gowns and utility gloves used to protect personnel from blood and body fluids and chemical hazards. The main use of barriers is to control gross contamination and not prevent spread of every single microbe. As an example, some of the viruses are smaller than the microscopic pores in latex exam gloves and therefore have a probability of passing through the glove material. In this instance, one may safely infer that gloves are meant for reducing the amount of exposure to the viral particles of the body fluids and not to totally prevent contact with the virus. Therefore, hand-washing with an antimicrobial soap after removing gloves is necessary and pragmatic. With respect to dentistry, there has not been a single reported and accepted case of disease transmission linked to passage of viral particle through the pores in the gloves.
We need use “full PPE” (protective eyewear, mask, gown and gloves) when there is a potential for splash or spatter (use of air/water syringe, highspeed handpiece and/or scalers), or a potential for exposure to chemicals that could splash/spatter on the face or mucosa. Full PPE would include protective eyewear, mask, gown and gloves.
Area of Infection Control
INFECTION CONTROL IN THE CLINICAL AREA
In the clinical area, there are various surfaces which are sources of infection and need to be barried and they include :
1. Dental Unit Light handles
2. Dental Chair Head Rest
3. Dental Chair Arm Rests
4. Dental Unit controls including the Bracket Table
5. Hand-piece
6. Air/water syringe
7. X-ray unit
8. Radiovisuography equipments
9. Apex locators
10. Endosonic Ultrasonic Units
Work surface barriers
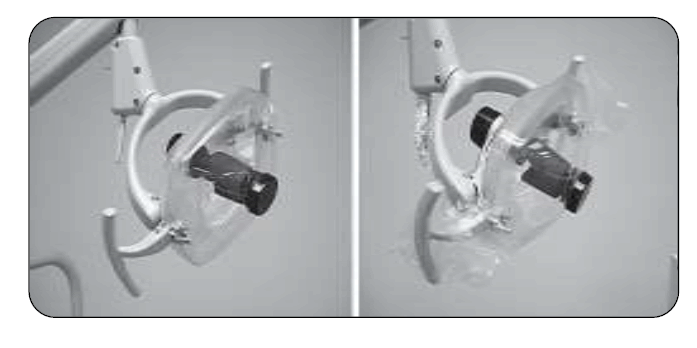
Light handles and light switches need to be barriered during patient use and discarded after each patient. Thin plastic bags, wraps or aluminum foil may be used

PRINCIPLES OF STERILIZATION
1. Dry heat kills the micro-organisms by :
❏ Denaturation of bacterial protein
❏ Oxidative damage
2. Moist heat kills the micro-organisms by : denaturation and coagulation of proteins
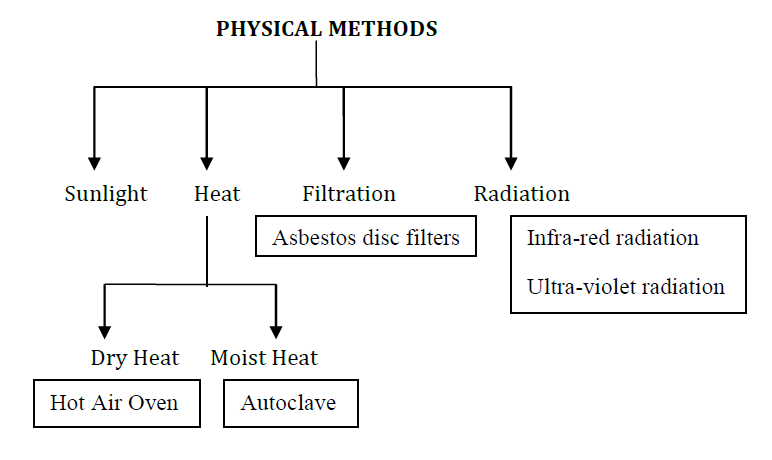
CLASSIFICATION OF STERILIZATION
Sterilization has been classified in two methods and they are as follows:
PHYSICAL METHODS
CHEMICAL METHODS
| Physical methods | Chemical methods |
|---|---|
| Incineration | Alcohols |
| Moist | Aldehydes |
| Dry heat | Halogens |
| Filtration | Phenols |
| Ionizing |
The physical methods of sterilization include – incineration, moist heat, dry heat, filtration and ionizing radiation.The chemical methods include – alcohols,aldehydes,halogens and phenols.
(Source : Bailey and Scott’s Diagnostic Microbiology 10th Edition pg.no.20)
CLASSIFICATION OF STERILIZATION
CHEMICAL METHODS
❏Alcohols - Ethyl Acohol
❏Aldehydes - Glutaraldehyde
❏Phenols - Cresol
❏Halogens - Chlorine
❏Dyes - Acridine
❏ Gases - Formaldehyde
(Source : Ananthanarayan & Paniker’s Textbook of Microbiology 8th Edition 2009 pg.no. 30-38)
STERILIZATION AND ITS METHODS
Most commonly used methods of sterilization includes :
I. Steam Pressure Sterilization (Autoclave)
II. Chemical Vapor Sterilization (Chemiclave)
III. Dry Heat Sterilization (Dryclave)
IV. Ethylene Oxide Sterilization
(Source : Sturdevant’s Art & Science of Operative Dentistry 4th Edition pg.no.371-380)
I. Steam Pressure Sterilization (Autoclave)
Principle of sterilization
When the steam comes in to contact with a cooler surface, it condenses to water and liberates it’s latent heat to that surface. The condensed water produces moist conditions for killing the microbes present
Sterilizing conditions
❏ Temperature : 1210c
❏ Pressure : 15 lb per square inch
❏ Time : 15 minutes
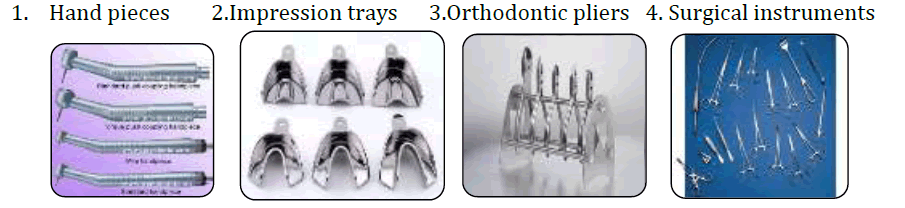
Instruments which are sterilized by using autoclave
There are various instruments which are sterilized by using autoclave. Some of them are as follows :
TYPES OF AUTOCLAVES
There are two types of autoclaves. They are :
1. Pre-Vacuum Autoclaves (Porous load autoclaves)
2. Gravity Displacement Autoclaves (Small portable bench model type autoclaves)
1. Pre-Vacuum Autoclaves (Porous load autoclaves)
In this type of autoclaves, the air which is present in the chamber is evacuated by the vacuum suction. They are used in Central Sterile Supply Units in hospitals. The sterilizing conditions – 121degree celsius at 20psi for 20minutes.They are used for the sterilization of suture materials, towels used for draping, cotton rolls and rubber gloves.
2. Gravity Displacement Autoclaves (Small portable bench model type autoclaves)
Principle
They work on the principle of downward displacement of air as a consequence of steam entering at the top of the chamber
❏ The sterilizing conditions are - 136 degree celsius at 32 Ib psi for 5 minutes
Advantages of autoclaves
The advantages of autoclave are :
❏The results are consistently good and reliable
❏ It’s time efficient
❏ It has a good penetration
Disadvantage of autoclave
❏ Blunting and corrosion of sharp instruments
II. Chemical Vapor Pressure Sterilization (Chemiclave)
Sterilization by chemical vapor under pressure is performed in a chemiclave. Chemical vapour pressure sterilizers operate at 2700 F (1310c) and 20 pounds of pressure. They are similar to steam sterilizers and have a cycle time of approximately half an hour.

Instruments which are sterilized by using chemiclave are :
❏Periodontal, restorative and endodontic instruments
❏ Carbon steel and other corrosion sensitive burs and pliers
Advantage of chemiclave
❏ Instruments are sterilized without rust or corrosion
Disadvantage of autoclave
❏ Items sensitive to the elevated temperature will be damaged
III. Dry Heat Sterilization(Hot Air Oven)
It is the most widely used method of sterilization by dry heat. The oven is electrically heated and is fitted with a fan to ensure adequate and even distribution of hat air in the chamber. It is also fitted with a thermostat that maintains the chamber air at a chosen temperature.
Sterilizing Conditions
❏ Temperature : 1600 c
❏Time : 2 hours
Instruments which are sterilized by using hot air oven are :
❏ Endodontic instruments
❏ Condensers
❏ Hand instruments
❏ Orthodontic pliers
❏ Surgical instruments
❏ Burs
Advantages of hot air oven
1. It does not cause rusting of instruments
2. It is relatively low cost of equipment
Disadvantages of hot air oven
1.It is time consuming
2.It is less effective and causes less penetration in the instruments
IV. Ethylene Oxide sterilization
Ethylene oxide sterilization is the best method for sterilizing complex, heat sensitive instruments and delicate materials.
Ethylene oxide is a gas at a temperature above 10.80c. It is highly explosive and inflammable. It is highly penetrative, non-corrosive agent with a bactericidal action. It is used for the sterilization of towels, metal and plastic instruments.
Sterilization in orthodontics
The instruments which are sterilized by using autoclave in orthodontics are :
❏ Orthodontic Pliers
❏ Scalers
❏ Banding and Bonding instruments
❏ Bands
❏ Impression trays
Further, plastic items which are used in orthodontics that cannot be autoclaved are placed overnight in Procide, an immersion sterilization solution.
❏ Procide is a Dental steriliant and is a buffered glutaldehyde solution
❏ It is re-usable for up to 28 days
❏ It is recommended for the sterilization of heat sensitive, immersible dental equipments and instruments Sterilization in Oral Surgery
The instruments which are used in oral surgery and are sterilized by using autoclave are :
▪ Periosteal Elevators
▪ Retractors
▪ Tissue Forceps
▪ Scissors
▪Needle Holders
▪ Surgical Curettes
▪ Bone Files
▪ Elevators
▪ Luxation Blades & Periotomes
▪ Extraction Forceps
Sterilization in Endodontics
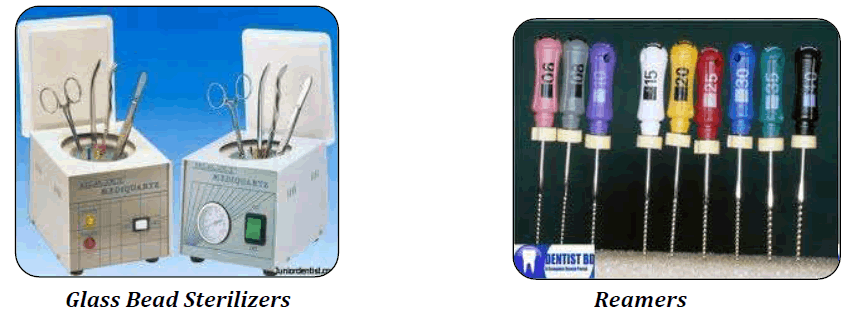
Glass Bead Sterilizer or Hot Salt Sterilizer
Absorbent points, broaches, files and reamers and other root canal instruments should be sterilized immediately before use in a hot salt sterilizer. This type of sterilizer is indispensible for endodontic work. The apparatus itself is compact as well as efficient. It consists of a metal cup in which table salt is kept at a temperature between 4250F (2180c) and 4750F (2460c).A suitable thermometer should be inserted in the salt at all times, if one is not incorporated in to the unit, so the temperature can be checked at a glance. At this temperature, root canal instruments such as broaches, files and reamers may be sterilized in 5seconds and absorbent points and cotton pellets in 10seconds.
The advantage of the hot-salt sterilizer lies in the use of ordinary table salt, which is readily available for replacement, instead of beads and eliminates the risk of clogging the canal.
Glass beads may be effectively substituted for the salt in a hot-salt sterilizer, provided the beads are less than 1mm in diameter. Larger beads are not so effective in transferring heat to endodontic instruments because of the larger air spaces between the beads that reduce the efficiency of the sterilizer.
Gutta Percha Cones
To sterilize a gutta-percha cone one should immerse the cones in 5.2% Sodium Hypochlorite for 1 minute then rinse the cones with Hydrogen Peroxide and dry it between 2 layers of sterile guage.

• Dappen dishes may be sterilized just before use by swabbing thoroughly with tincture of thimerasal followed by alcohol.Such swabbing can be done under pressure with the intent of physically removing debris and micro-organisms attached to the glass surface.
• Long handle instruments, tips of cotton pliers, blades of scissors and other instruments used in the course of an endodontic operation may be sterilized by dipping the working point in alcohol and flaming twice. Isopropyl alcohol may be used for this purpose but alcohol-formalin (3:1) is preferable.
NOTE : Thimerosal is an ORGANOMERCURIC COMPOUND. It contains 49.6% Mercury which is organically bound. It is an antiseptic and antifungal agent.
• The trade name of Thimerosal is MERTHIOLATE
• It is used as a preservative for vaccines,immunoglobulin preparations, skin test antigens
Sterilization in prosthodontics
The instruments which are used in prosthodontics that are sterilized by using autoclave are :
❏ All stainless steel, tungsten carbide and teflon-coated dental hand instruments
❏Burs
❏ Air-water syringe tips
❏ High-volume evacuator tips
❏ Metal impression trays
Sterilization in periodontics
The instruments sterilized by using autoclave in periodontics are :
❏ Ultrasonic periodontal scalers and tips
❏ Electro-surgery tips
NOTE
DENTAL ULTRAVIOLET STERILIZER

❏ They are provided with 12 number of trays made of stainless steel and are available in various specifications
❏ It emits light, and kills all the germicides. It is an ideal tool for avoiding contamination of instruments, once sterilized.
❏ Dental Ultraviolet Sterilizer, is completely safe as it ensures zero emission of UV light to avoid any harmful effect on the operator
❏ Dental equipments are sterilized by Dental Ultraviolet Sterilizer
COLD STERILIZATION
❏ Is a process in which sterilization is carried out at low temperature with the help of chemicals, radiation and by all other means except high temperature
❏ Sterilization by Ionizing radiations such as X-rays, Gamma rays, Cosmic rays is referred to as COLD STERILIZATION.
HOT WATER STERILIZER
❏ It is used in dental camps in mobile dental unit for sterilizing the used dental instruments and also used in dental clinical settings.

Disinfection and its methods
1. Alcohols
❏ Ethyl alcohol and Isopropyl alcohol are most commonly used alcohols
❏They are used as skin antiseptics
❏Oral pathologists use ethyl alcohol for the preparation of cytologic smears.
❏Disinfection of dental instruments
2. Aldehydes
Formaldehyde
❏ It is used for the fumigation of operation theatres

Fumigation Procedure
The steps involved in fumigation procedure are as follows :
1. Thoroughly clean windows, doors, floor, and all washable equipments with soap and water.
2. Close windows and ventilators tightly.
3. Switch off all lights, A/C and other electrical & electronical items
4. Calculate the room size in cubic feet (L×B×H) and calculate the required amount of formaldehyde
5. Formaldehyde is irritant to eye & nose; and it has been recognized as a potential carcinogen. So, the fumigating employee must use the personal protective equipments.
Fumigation methods
There are 2 methods of fumigation. They are :
I. Potassium Permanganate Method
II. Electric Boiler Fumigation Method
I. Potassium Permanganate Method
For every 1000 cubic feet, 450gm of Potassium permanganate (KMnO4) is added to 500 ml of formaldehyde (40% solution).Take about 5 to 8 bowls (heat resistant; place it in various locations) with equally divided parts of formaldehyde. This will cause auto boiling and generate fumes. After the initiation of formaldehyde vapour, immediately leave the room and seal it for at least 48 hours. After the fumigation process, neutralize the formaldehyde vapour with ammonia solution.
II. Electric Boiler Fumigation Method
For every 1000 cubic feet, 500ml of formaldehyde (40% solution) is added to 1000ml of water in an electric boiler. Switch on the boiler, leave the room and seal the door. After 45 minutes, switch off the boiler without entering in to the room (Switch off the main from outside).
3. Phenols
❏ Phenols exhibit bactericidal action
❏ The derivatives of phenol include – cresol, chlorhexidine, chloroxylenol and hexachlorophene. They are used as antiseptics.
4. Halogens
▪ Chlorine and Iodine – most commonly used halogens
❏Chlorine
- It is used in water supplies, swimming pools, food and dairy industries
- The derivatives of chlorine are Bleaching powder, sodium hypochlorite and chloramine
❏ Iodine
It is used as skin disinfectant. It is available in alcoholic and aqueous solutions
5. Betadine (Povidone Iodine)
- It is most commonly used in dentistry
- It is used as antiseptics
- It is used by the oral surgeons for disinfecting the skin prior to any surgical procedures
Public Health Significance
❏ Sterilization ensures patient safety, cost-effectiveness and prevents the spread of infectious diseases in the community.
❏As infection control program, even sterilization plays a significant role to “break the chain of infection” which will prevent the spread of infectious agent in the community
Conclusion
Sterilization is a process of killing all micro-organisms (including bacterial spores) in a material or object. Disinfection is the process of reducing the number of pathogenic micro-organisms. Sterilization and disinfection are achieved by using heat, filtration or chemicals. Overall, heat is the best means of sterilization Dry heat requires more time than moist heat The chemical families that provide useful sterilizing and disinfecting agents include alcohols, chlorine and iodine, phenols, aldehydes and ethylene oxide. An understanding of sterilization is essential for all dental personnel. It helps the health professionals to understand the need for careful compliance with recommended infection control protocols. The ultimate objective is to protect the patients, professionals and paraprofessionals.
References
- Anil Kohli, Raghunath Puttiah Infection Control and Occupational Safety Recommendations for Oral Health Professionals 2007
- Sturdevant’s Art & Science of Operative Dentistry 4th Edition pg.no.371-380
- Grossman Endodontic Practice 11th Edition pg.no.136-141
- Neelima Malik Textbook of Oral and Maxillofacial Surgery 1st Edition 2002, pg. no. 70-73
- Ananthanarayan & Paniker’s Textbook of Microbiology 8th Edition 2009, 30-38
- Shafer’s Textbook of Oral Pathology 6th Edition, pg .no. 922-925
- INTERNATIONAL JOURNAL OF DENTAL CLINICS VOLUME 3 ISSUE 1 JANUARY- MARCH 2011 Sterilization Methods in Orthodontics - A Review
- Sterilization Of Operation Theatre Using Fumigation Procedure ... www.getbestodds.info/44-sterilization-of-operation-theatre-using-fu..
- www.skdent.net/uvchambers.html
- Bailey and Scott’s Diagnostic Microbiology10th Edition pg.no.20
- Alcomo’s Fundamentals of Microbiology 8th edition pg. no.697
- Lakshman Samaranayake Essential Microbiology for Dentistry 3rd edition pg.no.319
- www.wikipedia.com
Citation: Suvarna V Biradar, Sterilization in Dental Practice – A Review, Asian Journal of Pharmaceutical Technology & Innovation, 6 (27); 53-66, 2018. www.asianpharmtech.com.
